Health Equity and Corporate Governance in Health Care Organizations: Challenges, Risks, Resources, and Strategic Responses
- May 23, 2022
- Almeta Cooper , The AECooper Group
- Michael Peregrine
ABSTRACT: Oversight of health equity in the delivery of quality medical care is the primary responsibility of health care organizations’ governing bodies. Failure to make it a priority could result in a breach of the duty of care and oversight by the health care organization. The number and breadth of challenging crises affecting the health care ecosystem of hospitals, health systems, health care professionals, and payers beginning in January 2020 has been unprecedented. Health equity, with its direct impact on racial and social justice, continues to be at the forefront of these critical challenges. Whether in health care or the broader context of Environmental, Social, and Governance Issues, health care organization governing bodies have been required to expand their understanding of the nature and context of health equity as they grapple with its impact on their clinical and business operations. Such understanding is required to examine the continuum of meaningful governance actions relative to health equity and to identify useful guidance and resources that will help governing bodies set organization goals and standards in a rapidly evolving environment. This article seeks to provide clarity and focus as leaders face challenges and risks, identify resources, and define their strategic responses to providing quality care.
Introduction
Health care organizations have been overwhelmed by a confluence of national crises related to social justice, systemic racism, a global pandemic, economic volatility, and a myriad of political crises, especially during the period beginning around January 2020. The impact of the sudden onset of these multiple crises—combined with their complexity and the profound uncertainty about the projected duration of their impact—was exacerbated by the concomitant disruption of day-to-day health care business operations and the delivery of quality medical care services. In this tumultuous environment, racial and social justice issues relative to health equity were exposed among the most challenging crises directly affecting the traditional U.S. health care ecosystem consisting of hospitals, health systems, health care professionals, and payers to name a few.
Specifically, governing bodies of health care organizations have been confronted with the impact of health inequities upon their core mission of delivering quality medical care services. Oversight of health equity in the delivery of quality services or conversely, detection of the existence of material health inequities, is the primary responsibility of the governing body. Failure to provide effective oversight could in some extreme cases result in a breach of the governing body’s duty of care to the organization and oversight responsibilities. Any governing body that does not understand the urgency of having meaningful processes in place to assure that health equity is included in the organization’s quality mission is at potential material, legal, regulatory, and reputational risk.
While coping with constantly changing circumstances in early 2020, governing bodies relied on their chief executive officers (CEOs) and general counsel as trusted advisors to assist them in fulfilling their responsibilities to lead the organization and set organization priorities. This was reflected in the “mission critical” core value of assuring the delivery of quality care despite the turbulence and uncertainties precipitated by the unprecedented confluence of national crises. The initial lack of and/or awareness of clear and cohesive legal, industry, regulatory, or policy guidance on health equity was even more disconcerting for board members expected to discharge their traditional fiduciary and mission critical oversight responsibilities. This void overwhelmed and paralyzed some governing bodies and sent their leadership teams scrambling to identify short-term solutions initially and later, longer-term solutions.
Apart from the multiple crises and lack of guidance that arose in connection with these extraordinary and unprecedented events, health care governing bodies were also affected by the public’s higher expectations of health care organizations and health care professionals to “do good” and “do no harm” to patients and their families. Concerns about reputational risk influenced the decisions of governing bodies, which have the ultimate legal and fiduciary responsibility for governing the health care organization. The reputational risk associated with the public’s expectations determines how or whether health equity and other social justice principles are proactively integrated within the organization’s core mission and business operations. Assuring the fulfillment of mission critical duties despite the uncertain state of the health care ecosystem is simultaneously an aspirational duty for health care governing bodies and a legal duty upheld in corporate governance cases decided by the Delaware Supreme Court.1 Importantly, the failure to preserve an organization’s reputation because of the existence of material health inequities could be considered harmful to the health care organization’s reputation, which is an asset of the organization that the governing body is obligated to protect.
The state of change in the health care ecosystem remains dynamic. Health care organizations’ governing bodies are strongly urged to monitor the proliferation of relevant federal and state government developments, publications, resources, and organization strategies that were made available in the second half of calendar year 2021. Notably, President Biden strongly signaled his policy commitment to equity for all, including health equity by addressing these subjects in two of the executive orders issued early in his administration. On January 20, 2021, he signed Executive Order 13985, Advancing Racial Equity and Support for Underserved Communities Through the Federal Government. On January 21, 2021, he signed Executive Order 13995, Ensuring an Equitable Pandemic Response and Recovery.2 These Executive Orders declared President Biden’s policy position:
It is therefore the policy of my Administration that the Federal Government should pursue a comprehensive approach to advancing equity for all, including people of color and others who have been historically underserved, marginalized, and adversely affected by persistent poverty and inequality. Affirmatively advancing equity, civil rights, racial justice, and equal opportunity is the responsibility of the whole of our Government.3
On August 30, 2021, the Biden Administration reinforced its commitment to health equity when it announced the creation of the Office of Climate Change and Health Equity (OCCHE) in the U.S. Department of Health and Human Services (HHS).4 The OCCHE is a novel federal approach to address climate change and health equity created in response to President Biden’s Executive Order 14008, Tackling the Climate Crisis at Home and Abroad.5 The Office’s mission is to protect communities that have been economically and socially marginalized, including communities that disproportionately bear the brunt of pollution and climate-driven disasters, such as drought and wildfires, at the expense of public health.
Governing bodies should monitor OCCHE’s activities and seek advice from counsel and senior management about its potential indirect and direct impacts on the health care ecosystem. An indicator of this philosophy was reflected in HHS Secretary Xavier Becerra’s response to questions about the reduction of carbon emissions from health care facilities: “We will use every authority to its greatest advantage because it is time to tackle climate change now.”6
This article is intended to be a resource for health care governing bodies, their CEOs, and general counsel to guide their organizations in (1) understanding the importance of language and concepts related to health equity, (2) identifying key areas of opportunity to integrate health equity in health care governing body actions pertinent to the delivery of quality care, and (3) identifying current guidance and resources. In addition, this article offers a forecast of potential future developments to monitor relative to health equity and makes recommendations about basic principles to consider when customizing the integration of health equity strategies in the core quality mission.
Understanding the Vocabulary of Health Equity, Health Justice, Health Disparities, and Health Inequities
Helping health care governing bodies understand what health equity means conceptually and how to distinguish health equity from other terms, such as health disparities and health justice, is a logical first step to adopting an organizational strategy. General counsel and/or board professionals charged with orienting health governing bodies and boards of directors often devote significant orientation time to familiarizing board members with traditional health care jargon, including technical and scientific terms, acronyms, and other specialized health care vocabulary. It is worth noting that health equity is not a new concept. Thought leaders in government, academic medicine, and frontline community organizers have been engaged in developing definitions of and strategies around health equity in the 1990s and earlier.7
A significant difference between the 1990s and 2020 health equity discussions is health care leaders in 2020 were confronted with the unprecedented and disproportionate impact of COVID-19 on certain populations, including people of color and the elderly.8 The pandemic exposed weaknesses in the health care delivery system, and the media and public demanded to know why those disparities existed. The pressure for answers heightened the need for a response by government and political leaders, as well as health care governing bodies, and under such pressure did it become apparent that more work needed to be done. Prior to 2020, health equity was not likely to have appeared as a recurring board agenda item for many health care organizations. If it appeared at all, it was probably no more frequently than annually.9
The term “health equity” is commonly used in health care and has been in use since at least the early 1990s; however, it is often not well-defined and is therefore used interchangeably with related terms, such as health disparities and health justice, which adds to the confusion about the concept of health equity.10 The American Medical Association (AMA) and the American Association of Medical Colleges Center for Health Justice joined together to publish an important and comprehensive resource, Advancing Health Equity: A Guide to Language, Narrative and Concepts11 (AMA-AAMC Advancing Health Equity Guide). The guide is intended to stimulate critical thinking about language, narrative, and concepts, many of which are ingrained in this nation’s culture and hinder the advancement of health equity. This seminal work clarifies commonly used definitions of health equity that follow below.
Reframing and rethinking the language and the underlying concepts used in addressing health equity and health inequity creates possibilities for reimagining health interventions; it shifts the focus from the personal/behavioral to the structural.12 Importantly, when the governing body possesses the language, tools, and understanding of health equity, it can effectively discharge its duty to oversee the existence of health equity in its operations and services.
Any one of the following four definitions, among the many alternatives, accurately conveys the meaning of health equity and can be useful as a standalone definition or in combination as a governing body learning resource:
- Dr. Camara Jones, former president of the American Public Health Association and physician and scholar, defines health equity as “the assurance of the condition of optimal health for all people.”13
- Dr. Paula Braverman’s expanded definition is consistent with Dr. Jones’ frequently cited definition: Health equity is the principle underlying a commitment to reduce—and ultimately eliminate—disparities in health and in its determinants, including social determinants. “Pursuing health equity means striving for the highest possible standard of health for all people and giving special attention to the needs of those at greatest risk of poor health, based on social conditions.” (emphasis added)14
- Further, Robert Wood Johnson Foundation’s 2017 report, What is Health Equity? defined health equity this way: “Health equity means that everyone has a fair and just opportunity to be as healthy as possible. This requires removing obstacles to health such as poverty, discrimination, and their consequences, including powerlessness and lack of access to good jobs with fair pay, quality education and housing, safe environments, and health care.”15
- A fourth and frequently referenced definition of health equity appeared in the Healthy People 2020 report issued by HHS: “[A]ttainment of the highest level of health for all people. Achieving health equity requires valuing everyone equally with focused and ongoing societal efforts to address avoidable inequalities, historical and contemporary injustices, and the elimination of health and health care disparities.”16
- Finally, the AMA’s definition of health equity is grounded in AMA policy: “Health equity, defined as optimal health for all, is a goal toward which our AMA will work by advocating for health care access, research, and data collection; promoting equity in care; increasing health workforce diversity; influencing determinants of health; and voicing and modeling commitment to health equity.”17
Health Equality vs. Health Equity
Health equity is not the same as health equality. These two terms are related and sometimes are used interchangeably. However, they should not be used interchangeably because health equality means everyone is given the same health care resources. The equal distribution of resources only has an equity outcome when everyone has the same needs. It is easier to appreciate the distinction between health equity and health equality with the visual representation depicted in the Equality-Equity graphic on page 81, which illustrates the difference between the two terms more quickly than words alone can. The graphic illustrates that “[t]o equalize opportunities, those with worse health and fewer resources need more efforts expended to improve their health.”18
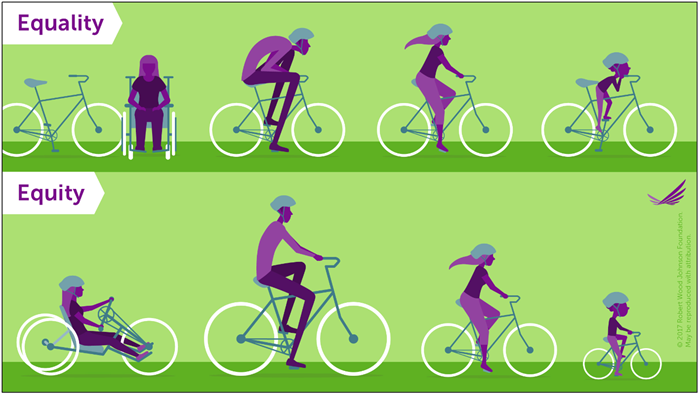
© 2017 Robert Wood Johnson Foundation
Health Inequities and Health Disparities
The term “health inequities” is identified in the AMA-AAMC Advancing Health Equity Guide as the preferred term to the commonly used term “health disparities,” which is explained as follows:
By health inequities, we mean gaps that are ‘unjust, avoidable, unnecessary and unfair’ . . . . They are neither natural nor inevitable. Rather, they are produced and sustained by deeply entrenched social systems that intentionally and unintentionally prevent people from reaching their full potential. Inequities cannot be understood or adequately addressed if we focus only on individuals, their behavior or their biology . . . . We have the opportunity—and the obligation—to do better, and to achieve more equitable outcomes. We believe that a critical component of that effort involves a deep analysis of the language, narrative and concepts that we use in our work.19
Health disparity has been used interchangeably with health equity. Although related to health equity, health disparity does not have the same meaning as health equity. “Health disparities reflect differences in health status between populations . . . . Health disparities adversely affect groups of people who have systematically experienced greater obstacles to good health based on their race, ethnicity, religion, socioeconomic status, gender, age, mental health, disability, sexual orientation or gender identity, or other characteristics historically linked to discrimination or exclusion.”20
These factors or determinants are the metrics used to assess the extent of health equity and how it changes over time for different groups of people.21 These primarily non-health factors or determinants of health status are currently, and with increasing frequency, referred to as either the social or political determinants of health. The social determinants include such factors as “income or wealth, education, neighborhood characteristics, or social inclusion—that people experience across their lives.”22 The political determinants of health include such factors as voting, government, and policy.23 A health disparity, in theory, can be avoided if scientific knowledge exists to potentially reduce or eliminate it and if resources were allocated to do so.24
Health Justice
The term “health justice” is a relatively new term and combines the concepts of health equity and social justice. In 2015, Professor Emily Benfer advocated for the “creation of ‘health justice’ [as] a new jurisprudential and legislative framework for the achievement and delivery of health equity and social justice.”25 The underlying concept of the term is that a mechanism should exist to allow health equity and social justice to form an “interdisciplinary and interprofessional response that engages all fields of expertise, including law, medicine, public health, social work, organizing, communications, historical studies, urban planning, education, and business, among others.”26 The ultimate goal of health justice is to protect the health of low-wealth people and people of color, as well as the fundamental liberty rights of all people.27
The Kinship of Environmental, Social, and Governance Issues to Health Equity
If one acknowledges the context of the emerging spotlight on health equity and its definition, including its emergence as an organizational priority, one can better understand why the definition of health equity is central to understanding the relationship between corporate governance and health equity. It is worthwhile to note that outside of health care, and similar to health equity’s elevation to a governing body level responsibility, governing bodies of public and private companies have experienced the elevation of Environmental, Social, and Governance (ESG) issues. ESG at one time was not generally perceived to belong in the governing body’s domain and more likely viewed as the responsibility of human resources, compliance, public relations, investor relations, or other departmental functions.28 However, over time, investor and public focus on ESG issues and their relationship to business operations and corporate success has made ESG issues more important, transforming them from “nice-to-do” aspirations to business-critical issues that require governing body attention.29 An in-depth examination of ESG is beyond the scope of this article, but most would agree that the umbrella of social justice issues covers health equity and that health care governing bodies can benefit from monitoring and learning from the ESG journeys of public and private companies.
Health Equity: The Journey Towards Meaningful Health Care Governing Body Actions
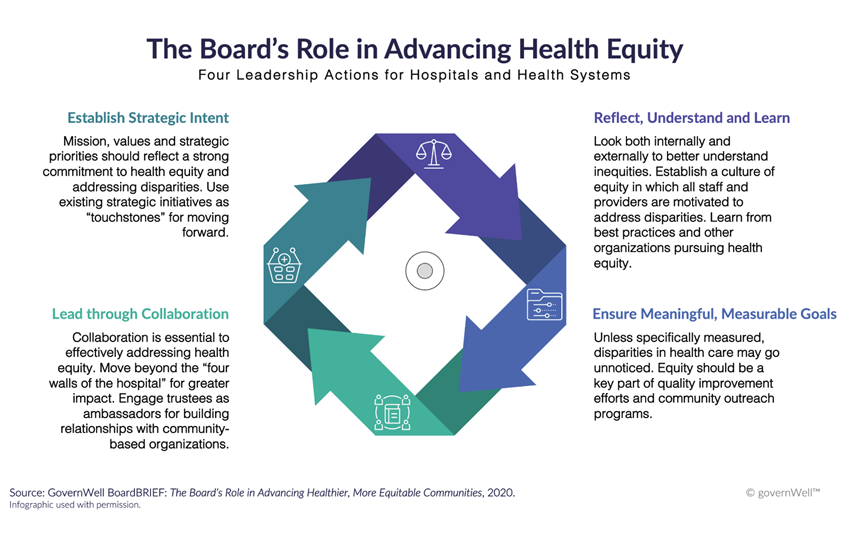
Many governing bodies start with educating themselves about the definition of health equity as a major first step in their health equity journey. The term “journey” is an important concept in this process because it connotes movement; the process is dynamic rather than static. The next step is identifying actions along the continuum of meaningful actions that the governing body can take to make impactful change. The following are examples of such actions:
- Declaration of a Commitment to Health Equity. A board has many options as to how the organizational commitment to health equity will be accomplished and communicated. As a board begins its journey to take meaningful action, it should consider how it can clearly articulate and communicate its position on health equity throughout the organization, from its leaders to managers, supervisors, employees, health professions staff, vendors, contractors, students, residents, patients, caregivers, families, and the community-at-large. The governing body may issue a formal statement, adopt or modify existing policy, modify its governance documents (bylaws) and/or incorporate principles, and adopt the language of health equity in some or all of its operations and throughout its organizational culture.
Governing bodies are cautioned that a beautifully written commitment to health equity alone is not sufficient to firmly establish health equity as a part of the corporate culture. Hollow statements can lead to backlash and weaken the trust relationship between the health care organization and its most important stakeholders, as well as harm the organization’s business operations.30 There must be a commitment from the top, i.e., from the governing body and executive levels along with allocation of adequate human, institutional, and financial resources. - Structure for Implementing and Monitoring Health Equity. How a health care governing body incorporates health equity principles into its governance structure will vary. Some will begin their health equity journey by training and educating first the governing body, followed by the executive team, management team, health professional staff, employees, residents, students and eventually, all relevant stakeholders.
Often, after a public health equity solidarity statement is issued, the next step is hiring an individual with primary oversight for health equity and diversity and inclusion. These positions are named according to the health care organization’s culture and structure. For example, some common titles are Chief Diversity and Inclusion Officer, Chief Health Equity Officer, or Chief Diversity, Inclusion, and Belonging Officer. The person holding this title typically reports to the health care organization’s CEO and has access to the governing body. This person’s success depends on adequate funding and staff.31
Some governing bodies have added health equity as a standing agenda item requiring regular reporting, similar to the reporting that is done for quality or compliance. Rather than adding a separate agenda item, some governing bodies have added health equity as a metric to existing reporting systems. Other governing bodies have established special committees or task forces to oversee the health equity activities implemented by management and to track the progress being made towards achieving the agreed-upon objectives and goals.32 Others have added health equity to reporting mechanisms that broadly address diversity and inclusion. As mentioned earlier, how a health care governing body incorporates health equity principles into its governance structure will vary. The path it chooses is not as important as its effectiveness for the organization. When it comes to structuring, implementing, and monitoring health equity efforts, it will be critical to embrace the message that “one size does not fit all.” - Governing Body Composition. Some governing bodies are re-examining their requirements for membership, due in part to the heightened focus on health equity and broader concerns with social justice and community needs. This examination includes scrutinizing the requirements that determine the existing governing body’s composition, asking whether these requirements perpetuate barriers to expanding diversity of thought, requiring consideration of diverse candidates, modifying term limits, and modifying geographic restriction requirements in order to more accurately reflect the patient population.33
The most prominent change in composition for many governing bodies is the intentional and immediate inclusion of diversity as the basis for selecting potential candidates for membership. A successful search begins with a process that requires a varied of pool of candidates, including those who are Black, Latino, Indigenous persons, Asian Americans, Pacific Islanders, other persons of color, lesbian, gay, bisexual, transgender, and queer (LGBTQ+) persons, or persons with disabilities.
The implied expectation from these changes is they will facilitate sensitivity and appropriate responsiveness to health equity issues. Another intended result is the stimulation of diverse thoughts. Refreshing the governing body’s composition—prompted by diversity, equity, and inclusion—may also cause the governing body to examine more broadly its needs in emerging health care priority areas, such as cybersecurity, population health management, or change management.
However, diversifying the governing body’s composition without being mindful of meaningfully including the new members will hinder their successful integration. Genuine and conscious inclusion of a new member is mutually beneficial to the individual and the governing body. Inclusion is most achievable when the governing body fosters a culture that is welcoming, respectful, and open-minded. More importantly, the governing body must assure that relationships among its members are based on collaboration and trust.34 - Financial Commitment. A governing body’s financial commitment to health equity is straightforward. A clear indicator of the board’s commitment to health equity is the existence of adequate funding that is allocated to implement the board’s stated commitment. This financial commitment will be evident in the organization’s annual budget, support of philanthropic and community initiatives, and financial incentives, if any, for employee performance, especially at the executive level. The goal is to support the health care organization’s commitment to health equity by linking compensation and performance to financial incentives.
- Board and Community Collaboration. Health care organizations that provide medical care are, by their nature, typically service organizations. Traditionally, they have sought community business leaders to serve as governing body members. However, they have not typically sought membership and direct participation from grassroots community leaders, which is a key stakeholder group. As a practical matter, the governing body for a health care organization should involve representation from key stakeholders who have frontline knowledge of the health equity concerns in the community served. It is noteworthy that non-profit hospitals already engage in a regular Community Health Needs Assessment (CHNA) every three years. Governing bodies should consider taking advantage of this valuable resource when adopting a health equity implementation strategy.35 The process of completing a CHNA should provide a governing body with specific information about the community it serves, including input from a cross-section of the community about its unique health needs. Accordingly, a governing body’s members should familiarize themselves with the content of the CHNA and ask questions when they arise.
Another useful resource to help governing bodies understand the benefits of community partnership is the National Academies of Sciences, Engineering, and Medicine 2017 report, Communities in Action: Pathways to Health Equity (2017 Communities in Action).36 The report takes a deep dive into the complexity of multiple factors that affect a community’s efforts to promote health equity, such as the actions that a community’s varied stakeholders must take or support. The report provides nine examples of geographically diverse communities that have programs and strategies that promote health equity. As noted in the report, limited media attention is given to community action that centers around health equity, in contrast to media attention that is often given to crime or community unrest.37
Assuming that adequate evidence can be collected to support the pursuit of high-level grassroots community collaboration, some leaders have experienced significant resistance to implementing such a strategy. The resistance has manifested itself primarily in the form of recommendations that community grassroots leaders be limited to acting in an advisory role. The rationale for such recommendations may be related to the concentration of highly educated individuals in health care and their misperception that community members’ lack of technical knowledge would be a significant barrier to effective governing body membership. However, with adequate training, orientation, and the help of knowledgeable facilitators, such perceived barriers can be overcome. This requires commitment, planning, and resources that will pay off with long-term gains in positive health outcomes. - Reputation, Patient Satisfaction, and the Business Case. Health care organizations, like other corporate entities, value their reputations. Health care governing bodies either expressly or indirectly view maintaining and enhancing their organization’s reputation as a top priority. Since the early 2000s, reputation has been inextricably tied to quality and consequently, the quest for high scores from Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS).38 Perhaps not surprisingly, health equity, at the time of this writing, had not been identified as a primary driver of reputation for a health care organization. However, there are indications that health equity has the capacity to offer a competitive business advantage to a health care organization.39 Specifically, having a reputation for effectively addressing health equity may help an organization “attract the best talent and elevate their brand and reputation” and “drive direct improvements to their mission to continually enhance the quality of care.”40 To the extent addressing health equity provides a competitive advantage and is viewed as part of the core health care value of quality, this advantage would in and of itself make a business case for treating health equity as a key commitment.41 From a purely dollars and cents perspective, investing in health equity may be expensive, but the reputational and long-term advantages are worthwhile. The 2017 Communities in Action report cited research that projected nearly $30 billion in savings during 2003-2006 had health disparities been eliminated from medical care in the U.S.42
On the other hand, a competitive advantage may become a disadvantage if a health care organization’s reputation becomes associated with discriminatory conduct because of denial of treatment that is consistent, systematic, fair, just, and impartial for all individuals. Health care organizations are not exempt from scrutiny if they elect to engage in “brand activism”43 and/or their leaders make public comments that are inconsistent with the institutional position. Many major corporations that issued statements during the height of social unrest in 2020 and the Black Lives Matter movement were later criticized for their inconsistent conduct.44 - Leadership: Chief Executive Officer, General Counsel, and Governing Body Chair. As with any important health care organization initiative, commitment at the highest level of the organization is critical for the initiative to be successful. Three key leaders and their support for the governing body are essential to the success of the organization’s commitment to health equity: the Chief Executive Officer, the General Counsel, and the Governing Body Chair. Practically speaking, most people readily accept the governing body’s ultimate legal oversight of the organization and that the governing body chair’s commitment and leadership is necessary to the success of any major organizational endeavor. Similarly, it is generally recognized that the CEO has primary responsibility for managing the organization’s operations at the governing body’s direction. How the CEO communicates and executes the organization’s health equity policies to external and internal audiences is critical to its integration into the organization’s culture. Finally, the general counsel’s position as a trusted advisor to the governing body and executive team makes him/her/them well positioned to help navigate the multi-faceted aspects of adopting health equity as part of the organization’s mission. Further, the general counsel is an excellent resource to respond to legal, legislative, and policy questions, and is particularly helpful with responding to questions not typically encountered by the governing body.45
Guidance and Resources
When health care organizations began seeking immediately accessible resources to help them formulate effective responses to the challenges associated with health equity, they reached out to their national professional associations and accrediting bodies. Many of the members of these governing bodies are also business leaders and/or serve on other public and private boards of directors, so they encouraged investigation into how public and private boards of directors in other sectors of the economy were responding. Health care associations, health care consultants, individual health care organizations, and health care thought leaders answered the call.
Among them, the American Health Law Association, American Hospital Association, American Medical Association, The Joint Commission, The Governance Institute, National Association of Corporate Directors, and Business Roundtable offer an impressive and expansive array of resources in every format to their members and/or the public. Collectively and individually, their resources provide a substantial foundation for any health care governing body to begin or advance its health equity journey. For example, they include introductory level materials,46 thought pieces,47 accrediting standards advisories,48 comprehensive white papers,49 guides and toolkits,50 strategic plans to guide members,51 guidance on the appointment of chief health equity officers and establishing health equity centers,52 and targeted resources to train and educate governing bodies. Commendably, these and other national organizations have provided reference materials and have convened thought leaders to share their collective knowledge and practical experiences to foster development of policy, stimulate problem solving, and identify best practices. For example, on April 12, 2021, the American Health Law Association convened a one-day virtual Convener on Racial Disparities in Health Care where eighteen health care experts engaged in a five-part focused discussion about health disparities and health equity.53 Convener participants tackled the definitions of health disparities and health equity, institutional decision making, equity in COVID-19 vaccine distribution, the social and political determinants of health, civic engagement, and potential solutions now and in the future. Two months later, on June 7-10, eight national foundations and other organizations sponsored a virtual Health Equity Summit comprised of over 100 concurrent and plenary sessions led by 250 national health equity experts. The significance of the scale and availability of these health equity-related resources is the dramatic contrast between the perceived dearth of resources and guidance available in early 2020 and the continually expanding availability of quality resources available in 2021 and beyond.
Health Equity in Action and Achievable Results
Inevitably, as part of a governing body’s discussion about health equity, the following questions will arise: What does health equity look like in our health care organization? With the uncertainty and economic pressures our organization is facing, how can we take on another initiative? What are examples of health equity best practices? Not every health care organization will have the financial resources to commit millions of dollars in the next decade to combat health disparities and racism while simultaneously advancing equity and inclusion internally.54 However, given the critical mass of available information that helps illustrate what health equity looks like in action at comparable organizations, every governing body can identify an impactful, practical pathway to integrate health equity into its existing programs, culture, and operations, some of which are referenced throughout this article.
Alternatively, another resource is programs that have received special recognition for their health equity strategies. Since 2018, the Centers for Medicare and Medicaid Resources (CMS) has given annual recognition to organizations that have demonstrated an exceptional commitment to health equity by reducing disparities and closing gaps in care among those they serve. Novant Health, one of the 2018 recipients, was recognized because of the actions initiated by a multidisciplinary team that discovered a disparity in pneumonia readmission rates. After conducting a root cause analysis, the team found connections between the discharge process, patient support after discharge, co-morbidities, and mortality rates. The team then developed targeted interventions for the discharge process, population health, and home visits. They created awareness and increased access to health care. Within one year, the disparity for Novant Health’s African American patients who were readmitted for pneumonia was reduced by 50% (from 4% to 2%) in comparison to other populations served. This effort was used as a blueprint to pursue other initiatives within Novant Health.55 The takeaway is that health equity can be achieved best by integrating it into a health care organization’s culture and tailoring the organization’s actions to meet the needs of the patient population it serves.
The Seattle Children’s Hospital Health Equity and Anti-Racism Action Plan (Plan) is another example of a comprehensive health equity plan.56 The Plan is the culmination of nine months of work that began in January 2021 when the hospital’s Board of Trustees created an Assessment Committee and charged it with overseeing and assessing its efforts to dismantle systemic racism and promote equity, diversity, and inclusion. The assessment was conducted by independent outside counsel, Covington & Burling, and led by former Attorney General Eric Holder. Next, the Plan was developed by a task force of diverse stakeholders and Seattle Children’s executive leadership. While it is too soon to evaluate the effectiveness of the plan, it is noteworthy because it incorporates many of the best practices used by other health care organizations in their journeys toward health equity. For example, the Plan is clearly supported by the Hospital’s governing body and executive leadership, many stakeholders were asked for their feedback, and the Plan was developed with their input. The Plan’s focus includes patients, their families, and the workforce; it has a defined timeline and specific health equity metrics linked to financial incentives, governing body participation, and is transparent in its communications regarding content and goals.
Forecast and Recommendations
As highlighted in this article, health care organizations and public and private companies initially responded to the national focus on systemic racism, social justice, and political unrest in the spring of 2020 with public statements of commitment to racial and social justice.57 Over time, the strategic responses developed by health care organizations and their governing bodies have been evolving beyond issuing general policy statements to identifying and implementing long-term solutions for systematically incorporating principles of health equity within their organizations. Also, health care organizations and their governing bodies have benefited from the ongoing generation and dissemination of practical policy guidance, as well as best practices that have become available from health care thought leaders.
Factors That Can Influence Forecast
Health equity does not exist in a vacuum. It is one of many issues in an expanding and long list of risks and issues confronting governing bodies in every sector of the economy, including health care.58 Achieving health equity has proved to be a long-term and complex process accompanied by significant challenges. Even the relatively recent acknowledgement of the significant impact that social and political determinants of health have on one’s access to health care has yet to eliminate the commonly held and mistaken belief that poor health results from “poor choices” and that people of color and low-wealth status should be convinced to make “positive choices” to alter their health outcomes. In addition, the prevailing attitude of political “short termism”59 hinders advancement toward achieving health equity. Adding to these challenges are the competing demands for allocation of resources and the unknown attention span of the general public to keep its focus on health equity as a priority, all of which make it difficult to forecast when health equity can be achieved.60
Another factor that could impact the forecast is the legal environment. Currently, express legal requirements mandating that governing bodies and health care organizations engage in specific actions to assure health equity do not exist. Legal advisors and/or general counsel should therefore continue to monitor for potential legal issues connected to health equity, such as employee relations or free speech.61 Similarly, the potential for legislative or regulatory activity as an indirect outgrowth of investor interest in diversity-related issues of public companies should be monitored. Large government-managed retirement funds in New York and California have asked public companies to publicly disclose their racial, ethnic, and gender composition of their workforce by publishing annual Employment Information (EEO-1) Reports in select job categories (e.g., New York City Comptroller’s Office and California Public Employees Retirement System). In addition, these government-managed retirement funds have urged state legislators to require public disclosure of such information. Activist investors such as Black Rock and State Street Global Advisors have also asked portfolio companies for public disclosure of racial and ethnic workforce composition.62
As mentioned earlier, President Biden issued Executive Order 13985 on Advancing Racial Equity and Support for Underserved Communities on January 20, 2021. Consistent with this policy, CMS subsequently sought and received comments on addressing significant and persistent inequities in U.S. health outcomes through improving data collection and in turn, better ways to measure and analyze disparities in its programs and policies.63
A potential outcome of this rule is the creation of a hospital equity score that should also be monitored by the health care organization’s general counsel. It is too soon to predict the full impact of the newly created OCCHE on CMS policies and its coordinated policy making with other federal agencies and departments; however, health care organizations and their general counsel should pay close attention to any rules or regulations issued, as well as their impact on the connection between health, health facilities, and climate change. This is another technical area in which governing bodies will have to expand their knowledge base and know-how.
Governing bodies have been required to make similar adjustments with other impactful disruptors, such as Artificial Intelligence, cybersecurity, and other technologies. All of these disruptors have health equity implications that will require thoughtful and creative strategies and solutions.
Economic, political, technological, and social justice pressures are ongoing, and they will compete with health equity for governing body attention. Governing bodies should therefore identify members who are equipped to lead in this effort and keep the institution’s focus on health equity. One may also anticipate that the business case for health equity will have to be strengthened given the economic pressures in health care that are ever present.
Recommendations for Developing a Health Equity Strategy
Health care governing bodies are strongly urged to consider these basic principles when tailoring their individual health equity strategies:
- The oversight of a health care organization’s core mission to equitably deliver quality medical care is the duty of the governing body.
- Given the complex and dynamic state of health care and the political and social determinants that impact one’s health and the health of entire communities, the goal of achieving health equity in the delivery of quality medical care is a journey. It will not be achieved with a “one and done” mentality.
- To be effective, health equity must be integrated into the organization’s goals, culture, and language. Effective health equity efforts will require a strategic plan of action, just like any other board-level organizational issue, and it must be an essential element of a living document that is capable of being adapted to accommodate emerging issues such as climate change and its impact on health equity. The plan of action should include standardized regular reporting of trends and outcomes, a reasonable timeline for implementation of the plan, and a clearly stated system of accountability and measurement.
- Health care organization outcomes and executive performance must be measured and tied to compensation and financial incentives.
- Active and inclusive leadership can be a powerful determinant in helping a health care organization achieve and advance its core mission of providing quality care and health equity.
Conclusion
The delivery of quality medical care, including the achievement of health equity, is mission critical for health care organizations. Implementing health equity-focused recommendations are part of a governing body’s important journey toward fulfilling that core mission. Notably, there has been an explosion of available health equity resources and commentary in 2021 that should be monitored and used to facilitate and enhance the organization’s journey. It is critical for all involved to remember the concept of the journey during this process that governing bodies must undergo to find ways that will effectively integrate health equity into their actions; the journey will be continually changing and dynamic. Most importantly, a governing body must not lose its focus on health equity as an essential component in guiding decisions and as an essential measure of quality.
Author Profiles
Almeta E. Cooper is a former president and Fellow of the American Health Law Association (AHLA). She serves AHLA in multiple roles, including as speaker, author, and co-editor of AHLA’s Journal of Health and Life Sciences Law Special Issue, “Emerging Issues in Health Equity in the United States: Legal, Legislative, and Policy Perspectives.” She also serves on various AHLA program planning committees and advisory committees. Almeta has served as general counsel and corporate secretary for hospitals, health systems, medical schools, and a state medical association. She currently focuses on regulatory analysis and public policy topics such as health equity and environmental justice. Almeta is the principal for The AECooper Group and provides executive advice to attorneys, small businesses, corporations, and nonprofits. In addition, she leads state level organizing on clean air and children’s health for Moms Clean Air Force, a national organization of more than 1,000,000 moms and dads. Contact her via email at [email protected].
Michael W. Peregrine represents corporations, their officers, and directors on governance and fiduciary duty matters, officer-director liability issues, charitable trust law, and corporate structure as a partner at McDermott Will & Emery. Michael is recognized as one of the leading national practitioners in corporate governance law and is a senior contributor to Forbes.com, where his articles focus on governance and leadership topics. He also authors regular columns on corporate governance-related topics for Agenda, CorporateCounsel.com, and publications for The Governance Institute and the American Health Law Association (AHLA). Michael is a co-author of the three corporate governance compliance white papers published jointly by the Office of Inspector General (Department of Health and Human Services) and AHLA. Michael is outside governance counsel to many prominent corporations, including hospitals and health systems, voluntary health organizations, colleges and universities, social service agencies, health insurance companies, pharmaceutical companies, and financial institutions. Contact him via email at [email protected].
1 See Marchand v. Barnhill, 212 A.3d 805 (Del. 2019). For a summary description about governing body mission critical oversight responsibility, refer to the 2021 National Association of Corporate Directors (NACD) report, “2021 Governance Outlook: Projections on Emerging Board Matters,” which highlights several Delaware Supreme Court corporate governance cases and the Court’s decisions trending toward holding governing bodies accountable for oversight of mission critical risks. NACD, 2021 Governance Outlook: Projections on Emerging Board Matters (2020).
2 Exec. Order No. 13995: Ensuring an Equitable Pandemic Response and Recovery, 86 Fed. Reg. 7193 (Jan. 21, 2021), https://www.govinfo.gov/content/pkg/FR-2021-01-26/pdf/2021-01852.pdf.
3 Exec. Order No. 13985: Advancing Racial Equity and Support for Underserved Communities Through the Federal Government, 86 Fed. Reg. 7009 (Jan. 25, 2021), https://www.govinfo.gov/content/pkg/FR-2021-01-25/pdf/2021-01753.pdf.
4 See Press Release, HHS, HHS Establishes Office of Climate Change and Health Equity (Aug. 30, 2021), https://www.hhs.gov/about/news/2021/08/30/hhs-establishes-office-climate-change-and-health-equity.html.
5 Exec. Order No. 14008: Tackling the Climate Crisis at Home and Abroad, 86 Fed. Reg. 7619 (Feb. 1, 2021), https://www.govinfo.gov/content/pkg/FR-2021-02-01/pdf/2021-02177.pdf.
6 Stephanie Armour, Climate Change to Be Treated as Public-Health Issue,
7 See, e.g., writings of Camara Jones, MD and Paula Braverman, MD, referenced in this article.
8 Brad Boserup et al., Disproportionate Impact of COVID-19 Pandemic on Racial and Ethnic Minorities, 86
9 Natalie Cooper et al., Board Practices Quarterly: Diversity, Equity, and Inclusion,
10 Paula Braveman et al., What is Health Equity?,
11 Am. Med. Ass’n, Advancing Health Equity: A Guide to Language, Narrative and Concepts (2021), https://www.ama-assn.org/system/files/ama-aamc-equity-guide.pdf; see Nat’l Ass’n Cnty. & City Health Offs. (NACCHO), Advancing Public Narrative for Health Equity & Social Justice (2018), http://publichealth.lacounty.gov/CenterForHealthEquity/PDF/advancing%20public%20narrative%20for%20health%20equity%20and%20social%20justice_NACCHO.pdf; Open Soc’y Founds., Building Narrative Power for Racial Justice and Health Equity (2021). In 2009, NACCHO received a two-year grant from the National Center for Minority Health and Health Disparities at the National Institutes of Health to create an educational website that helps public health practitioners recognize and act more effectively on the social injustices at the root of health inequity. The recommended content is available from the website as part of the course or as a handbook.
12 Am. Med. Ass’n, Advancing Health Equity: A Guide to Language, Narrative and Concepts 11 (2021), https://www.ama-assn.org/system/files/ama-aamc-equity-guide.pdf.
13 Sarah M. Tracey et al., Introduction to Health Equity and Social Determinants of Health,
14 Paula Braveman, What Are Health Disparities and Health Equity? We Need to Be Clear, 129
15 Paula Braveman et al., What is Health Equity?,
16 Off. Disease Prevention & Health Promotion, Disparities,
17 Am. Med. Ass’n, Advancing Health Equity: A Guide to Language, Narrative and Concepts 5 (2021), https://www.ama-assn.org/system/files/ama-aamc-equity-guide.pdf (citing Plan for Continued Progress Toward Health Equity H-180.944).
18 Paula Braveman et al., What is Health Equity?,
19 Am. Med. Ass’n, Advancing Health Equity: A Guide to Language, Narrative and Concepts 4 (2021), https://www.ama-assn.org/system/files/ama-aamc-equity-guide.pdf.
20 Priya Bathija, Addressing Health Equity in the Hospital Board Room,
21 Paula Braveman et al., What is Health Equity?,
22 Id. at 3.
23
24 Paula Braveman et al., What is Health Equity?,
25 Emily A. Benfer, Health Justice: A Framework (and Call to Action) for the Elimination of Health Inequity and Social Injustice, 65
26 Id.
27 Id.
28 Dave Curran & Krishna Veeraraghavan, Working ESG Into Your Board Playbook (Nov. 7, 2021),
29 Id.
30 See Fernando Duarte, Black Lives Matter: Do Companies Really Support the Cause?,
31 See Rob Kelly, The Top 20 Diversity Titles [with Descriptions],
32 See Tina Freese Decker, Leading Healthcare Towards Greater Health Equity,
33 NACD, Diversity and Inclusion Resource Center, https://www.nacdonline.org/insights/resource_center.cfm?ItemNumber=22875 (last visited Apr. 22, 2022).
34 See Pamela Knecht et al., Board Expertise and Diversity for the Future, 32
35 See IRS, Community Health Needs Assessment for Charitable Hospital Organizations – Section 501(r)(3), https://www.irs.gov/charities-non-profits/community-health-needs-assessment-for-charitable-hospital-organizations-section-501r3 (last reviewed or updated Aug. 3, 2021).
36
37 Id. (community agency to promote health equity).
38 See Hospital CAHPS (HCAHPS),
39 Kulleni Gebreyes et al., Activating health equity (Apr. 12, 2021), https://www2.deloitte.com/us/en/insights/industry/health-care/developing-an-agenda-of-equity-in-health.html.
40 Id.
41 An interesting inquiry beyond the scope of this article is how shall the competitive advantage of an established commitment to health equity in 2021 and beyond be measured during the so-called “Great Resignation,” a time when employers seem to be desperate to use all enticements to hire and/or retain employees at all levels of an organization.
42
43 See What is brand activism?,
44 Fernando Duarte, Black Lives Matter: Do Companies Really Support the Cause?,
45 Michael W. Peregrine, The Health Care Board Response to the Social Justice Environment (July 10, 2020), https://d1198w4twoqz7i.cloudfront.net/wp-content/uploads/2020/09/21181159/Weekly_Peregrine_071020.pdf.
46 See Priya Bathija, Addressing Health Equity in the Hospital Board Room,
47 See Anne Rooney & Barbara Lorsbach, The Board’s Role in Advancing Healthier, More Equitable Communities,
48 Joint Comm’n, Health Equity – General Resources (2016), https://www.jointcommission.org/-/media/tjc/documents/resources/patient-safety-topics/health-equity/health_equity; Joint Comm’n, Advancing Effective Communication, Cultural Competence, and Patient- and Family-Centered Care: A Roadmap for Hospitals (2010), https://www.jointcommission.org/-/media/tjc/documents/resources/patient-safety-topics/health-equity/aroadmapforhospitalsfinalversion727pdf.pdf?db=web&hash=AC3AC4BED1D973713C2CA6B2E5ACD01B&hash=AC3AC4BED1D973713C2CA6B2E5ACD01B.
49 NACD, Update of the Diverse Board Moving From Interest to Action: 2020 Blue Ribbon Commission Report (Dec. 17, 2020), https://www.nacdonline.org/insights/blue_ribbon.cfm?ItemNumber=68976.
50 See NACD, Board Oversight of Corporate DE&I Programs, in
51 See The AMA’s strategic plan to embed racial justice and advance health equity,
52 See Announcement of Aletha Maybank, MD, as first chief health equity officer of the American Medical Association who heads the association’s Center for Health Equity, established with accountable values and principles in April 2019. AMA’s Center for Health Equity mission and guiding principles,
53 Am. Health L. Ass’n, Equity in Health Care and Health Law Practice, https://www.americanhealthlaw.org/publications/health-law-hub-current-topics/dei-in-health-care/equity-in-health-care-and-health-law-practice (last visited Apr. 22, 2022). Both the AHLA Convener and the Virtual Health Equity Summit are archived and available to the public.
54 Jared Mueller, Driving Equity, Inclusion, and Diversity in Healthcare: A Discussion with Mayo Clinic’s Dr. Anjali Bhagra,
55 See Past CMS Health Equity Award Winners,
56 Seattle Childs., Health Equity and Anti-Racism Action Plan (2021), https://www.seattlechildrens.org/globalassets/documents/about/health-equity-and-anti-racism-action-plan.pdf.
57 See findings based on an August 2020 survey of members, representing more than 200 companies of the Society for Corporate Governance reflecting that 100% of the respondents had issued a statement to publicly acknowledge racial injustices or articulate the company’s position.
58 See Martin Lipton et al., Key Corporate Governance Issues at Mid-Year 2021,
59 Linden Farrer et al., Advocacy for Health Equity, 93
60 See EU based research referencing among other resources Robert Wood Johnson Foundation findings. Linden Farrer et al., Advocacy for Health Equity, 93
61 Michael W. Peregrine, The Health Care Board Response to the Social Justice Environment (July 10, 2020), https://d1198w4twoqz7i.cloudfront.net/wp-content/uploads/2020/09/21181159/Weekly_Peregrine_071020.pdf.
62 Nat’l Ass’n Corp. Dirs., Board Oversight of Diversity, Equity, and Inclusion to Combat Racism (2020).
63 Compare current policy with the 2015 report, Ctrs. for Medicare & Medicaid Servs., Off. Minority Health, The CMS Equity Plan for Improving Quality in Medicare (2015), https://www.cms.gov/about-cms/agency-information/omh/omh_dwnld-cms_equityplanformedicare_090615.pdf. Although the 2015 report limited its focus to Medicare recipients, it presented a viable strategy for reducing health care inequities using a framework of “improving [CMS’] understanding and awareness of disparities, their causes and why they matter; creating and disseminating promising solutions; and implementing sustainable actions . . . [CMS] will reach [CMS’] destination of reduced disparities and healthier Medicare beneficiaries.” Id. at 14.