Digital Health Equity: Narrowing the Digital Divide by Ensuring a Fair, Equitable, and Just Opportunity to Access Digital Health
- May 23, 2022
- Priya Bathija , American Hospital Association
- Sarah Swank , Nixon Peabody LLP
ABSTRACT: Since the onset of the COVID-19 pandemic, digital solutions, including mobile health apps, patient portals, and telehealth serve as a critical access point for health care providers to reach patients. Modifications of state and federal laws and regulations in response to the pandemic, such as licensure and reimbursement waivers, provided opportunities to expand care settings, including to the home, and increased the types of providers that could provide virtual care without being in person with the patient.
Digital solutions, however, have not been available to many. Barriers exist for meaningful access to these digital solutions across the country. The pandemic highlighted several of these barriers when the health care industry pivoted to remote care rather than in person visits. For example, the pandemic shone a light on barriers such as digital literacy; cultural competency; and inconsistent access to broadband/high-speed internet, cell service, and smartphones. Those individuals without access to these digital resources face challenges to meaningfully accessing or receiving care.
Attorneys and policymakers play a key role in addressing these challenges and have the opportunity to design and frame relationships between technology and providers and to advance broader policy changes to promote digital health equity. This article frames these legal issues and uses real life examples to highlight digital access and literacy challenges and opportunities. In addition, it sets forth the legal challenges at play and identifies specific actions attorneys can take to reduce the digital divide.
Introduction
When the COVID-19 pandemic began, health care providers dramatically increased the use of technology and digital solutions to deliver care. Office closures and cancelation of certain procedures due to public health concerns created a need for patients to seek care from health care providers outside of a clinical setting. Initially, delivering care virtually became a way to address shortages in personal protective equipment, respect social distancing guidance, reduce the spread of the virus, and manage, in certain geographies, large numbers of COVID-19 patients.
In the first months of the pandemic alone, research suggests that telehealth usage rose from less than one percent of visits to as much as 80% where COVID-19 prevalence was high.1 Throughout the year, telehealth usage continued across the country. A recent analysis conducted by Kaiser Family Foundation analyzing data from Medicare and Medicare Advantage found that 15 million (or just over one in four) Medicare beneficiaries had a telehealth visit with a doctor or other health professional between the summer and fall of 2020.2 As of July 2021, it was estimated that telehealth utilization had stabilized at levels 38 times higher than before the pandemic.3
Despite this increase in telehealth utilization, many individuals could not benefit from these solutions. These individuals either did not have access to the technology necessary or faced digital literacy obstacles to navigating, understanding, and communicating information through a digital format. As a result, they were essentially shut out of this new model of health care delivery. Telephonic backup became a safety net to digital solutions.
The COVID-19 pandemic has shown how crucial technology is for health care delivery. As we move forward, the health care system appears to support adoption of virtual care models and digital solutions, making digital health equity, including digital access and literacy, critically important. As health care providers design and implement digital solutions, it will be imperative to take proactive steps so all individuals have the opportunity to engage with these tools and use these digital solutions to access health and health care.
The following discussion explores what digital health equity is, current barriers to digital health equity, and practical tactics and solutions that may be used to improve digital health equity.
What is Digital Health Equity?
The best place to start is by understanding what health equity is and its relation to digital health equity. Health equity has been simply defined as the attainment of the highest level of health for all people.4 It has also been described as a situation in which everyone has a fair and just opportunity to be as healthy as possible.5
Digital health is broadly defined as the field of knowledge and practices associated with the development and use of digital technologies to improve health.6 Digital health equity is the fair and just opportunity to engage with digital health tools to support good health outcomes.7 This includes access to the technology needed to use mobile health apps, patient portals, and telemedicine. It also includes digital health literacy—the ability of a patient to obtain, process, and understand digital services and information.8
The lack of access to technology and digital health literacy can be categorized as a social determinant of health or a super determinant of health.9 It is important to acknowledge that both are societal factors that influence the health of individuals and communities. Lack of access to technology can have significant health consequences.10 Federal Communications Commission (FCC) data shows that in areas with lower broadband connectivity, residents have higher rates of obesity, diabetes, unnecessary hospitalizations, and sick days than national averages.11
In addition, lack of access to broadband and other technology can impact other factors that influence health—including the ability to apply for employment, housing, and other assistance programs that are increasingly accessible online.12 Moreover, as all areas of our lives become tied to technology and digital solutions, those without broadband will not have the same access to food, education, economic stability, and the ability to engage with others in their communities.
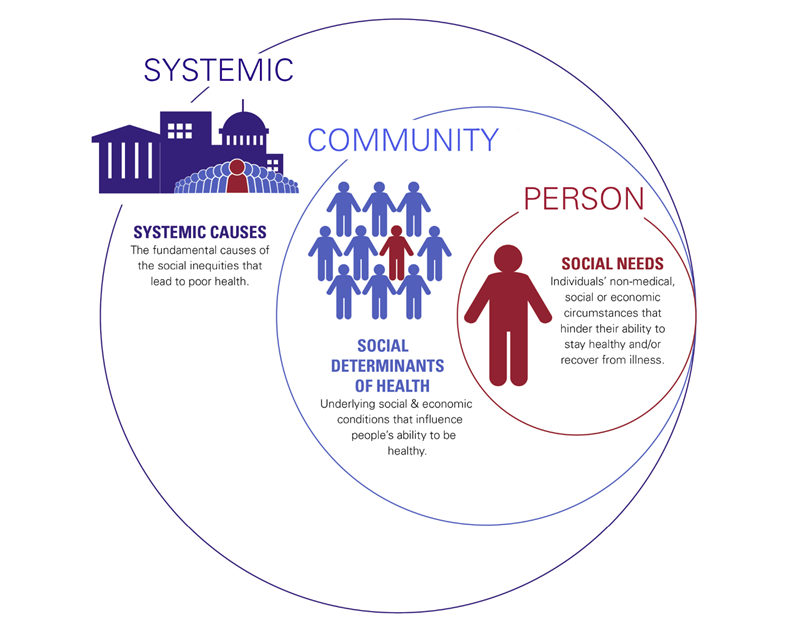
The American Hospital Association (AHA) has set forth a framework that explains how societal factors of health can be addressed at the individual, community, and systemic levels.13 When examining digital health equity, it can be addressed as a social need at the individual level, a social determinant at the community level, and as a systemic cause that is leading to poor health outcomes.
Societal Factors That Influence Health: A Framework for Hospitals
Current Barriers
There are millions of individuals across the country who lack either the technology or the digital health literacy needed to take advantage of digital solutions.
At the end of 2019, the FCC estimated that 14.5 million Americans lacked access to fixed broadband service at threshold speeds.14 While there have been gains in bringing high-speed broadband service to all Americans, a recent report from Microsoft estimates that 157.3 million Americans do not use the internet at broadband speeds.15
In areas where broadband infrastructure is available, there are millions of families that cannot afford to have broadband access.16 According to estimates from the U.S. Census, 13.9% of urban households and 19.2% of rural households do not have a broadband subscription.17 Racial and ethnic minorities, people living on tribal lands, older adults, and people with lower levels of education and income also are less likely to have broadband at home.18
In addition, access is further limited when individuals do not own the technology needed to operate these digital solutions. Many individuals still do not own smartphones. The Pew Research Center reports that 14% of individuals living in rural areas own a cellphone but not a smartphone.19 A recent study among Medicare beneficiaries found that over 40% of Medicare beneficiaries lacked a smartphone with a wireless data plan.20 As a result, these individuals cannot take advantage of mobile health apps, patient portals, or health care services offered through telemedicine.
Even with access to technology, the ability to use, process, and understand technology, or digital literacy, can be a barrier to access. For example, most available digital health tools are available in English only and are written at high reading levels.21 Therefore, individuals who do not speak English or who cannot read at greater than a 12-grade readability may struggle to comprehend the information in digital formats. Individuals may also face cultural barriers or lack the training or knowledge needed to use digital tools, computers, and smart devices.22
Legal Considerations Surrounding Digital Health Equity
Legal barriers and opportunities exist for digital health equity. Federal and state laws, as well as governmental value-based programs are starting to look at removal of these barriers to facilitate greater access to digital solutions. Certain access laws have been on the books. Yet the concept of navigating these laws through the lens of digital health equity is new. At the same time, new coding and data collection could create informed decisions on a provider level and inform policy and payment decisions in the future. Following are some legal considerations surrounding digital health equity.
Providing Technology Can Trigger an Analysis Under the Federal Fraud and Abuse Laws
Prior to the pandemic, traditional fee-for-service Medicare payment for telehealth was limited to certain rural areas and certain providers and did not reimburse many providers for care to patients in their homes. Effective March 6, 2020, through the declaration of a Public Health Emergency, emergency waivers (“1135 waivers”) and the Coronavirus Preparedness and Response Supplemental Appropriations Act of 2020 expanded payment under traditional Medicare beyond geographic areas, provider types, and locations of the provider and patient, including services in the home.23 During the pandemic, pilot programs and innovative care models also have expanded the use of technology to supplement the in-person care provided to patients that was not covered as reimbursable services prior to the pandemic.24 Yet not everyone has access to the resources they need in this new digital explosion in health care. Those considering addressing this need must review the federal and state fraud and abuse laws.
Hospitals and other providers might find that the provision of free technology is a simple solution to this problem. Yet under the federal fraud and abuse laws, the provision of free or more than nominal goods or services to a Medicare beneficiary can implicate the Civil Monetary Penalties Act (CMP). Although the CMP law allowed for the provision of certain goods or services if they promote access to care, the provision of free technology should be reviewed.25
In addition, the provision of free or less than fair market value goods or services to a physician from a hospital or others in the position to refer could implicate the Stark Law26 or the Anti-Kickback Statute.27 For example, a hospital may want to provide tablets to physicians for their own use or their patients’ use as part of a program of an identified high-risk population such as diabetes or asthma to ensure medication management. The provision of the tablet to a referring physician, however, could implicate the Stark Law or Anti-Kickback Statute for physicians and practice patients who are Medicare beneficiaries.
At the same time, value-based governmental programs such as Medicare Advantage or a capitated Medicaid program may allow or even require access to technology. One solution is to provide such technology just for Medicare Advantage, commercial payers, or managed care patients when permitted under contract. A payer-by-payer approach is not within the spirit of providing good care to Medicare beneficiaries and is not satisfying to care providers.
The idea of treating patients differently based on their payer category may not feel right to the health care providers who are treating these patients, but in itself could still implicate these federal fraud and abuse laws.
Further, a hospital’s provision of free technology of a high value to Medicare beneficiaries directly could implicate the Civil Monetary Penalties Laws.28 Loaner programs and other solutions can address these concerns but can create uncertainty around the fraud and abuse laws.29 In addition, the new Sprint Rules provide greater flexibility for care coordination services for value-based entities. This analysis assumes that patients have equal access to the hospital and physicians, along with the programs that would provide for such technology. The next question to ask is whether current access laws go far enough in promoting digital health equity.
Redefining Access in a Digital Age
Access laws are laws that promote the ability to obtain health care services in a health care setting. For example, the Office for Civil Rights (OCR) enforces federal civil rights laws and nondiscrimination regulations that apply to programs, services, and activities that receive federal financial assistance from the Department of Health and Human Services (HHS). These laws include, among others, discrimination based on race, color, national origin, disability, sex, pregnancy, sexual orientation, gender identity, and age.30
One such law is the Americans with Disabilities Act (ADA).31 In 2020, the ADA turned 30.32 The ADA was intended to remove barriers to physical access for those who have a disability, such as inaccessible facilities and equipment. It also includes enforcement provisions related to discrimination based on disability. These laws have implications in the digital world as well. Yet the digital world can create unique barriers perhaps unintentionally. For example, chat features, website functionality, and app functionality can create barriers to accessing care when care is accessed through a digital solution.
At the same time, access could be expanded for those who are disabled and other protected classes under these access laws. One idea is to review technology solutions and the provisions of access required in person and apply those elements to a virtual environment and access to electronic information technology (EIT). OCR notes that “covered entities must offer people with disabilities full and equal access to the EIT they employ, unless those individuals are provided reasonable accommodations or reasonable modifications that permit them to receive all the benefits provided by the EIT in an equally effective manner.”33 For example, interpretative services both under the ADA and for Limited English Proficiency Individuals (LEPs)34 could be embedded into a telehealth solution to ensure video interpretative services.35 Even if these solutions are embedded in technology, the functionality to access these services must allow the user to easily find and navigate them. Another example includes interpretative services for LEPs in a telehealth solution and its ability to easily select the user’s primary language so they can then access the interpretative services for their telehealth visit.36
A best practice is to conduct an access review, audit, and ensure ongoing monitoring of health care programs and care that includes updates to reflect a virtual health care setting. Hospitals and health care providers often maintain policies, procedures, reviews, and training for these practices, policies, and care protocols in the office, hospital, or other physician care setting to remove barriers for protected classes. These can be added to reflect a virtual care setting. This review, audit, and monitoring could include review and updates to: (1) access policies and procedures, (2) implement non-discrimination policies and protocols, including a patient bill of rights, (3) train physicians, employees, and contractors, (4) conduct customer services questionnaires and community outreach, (5) review of wait times for services, (6) collect data related to interpretative, language, or other needs, (7) review new patient or admission process and data collection, (8) add contract provisions and requirements for contractors to meet access standards, (9) recruit and retain physicians, clinicians, employees, and contractors that reflect the community served, and (10) consider a culturally competent navigation program that reflects community needs.
Data Collection
In a report to Congress, HHS cited telehealth services as a potential solution to address beneficiaries without access to transportation in order to create expanded access in Medicare’s value-based programs.37 The same report discussed the collection and use of social risk data in an effort to address patient needs. HHS’s second report to Congress in March 2020 went further and stated that, “[i]ncluding health equity measures can help providers prioritize areas for particular focus, and specific measures targeting equity within existing quality reporting programs can motivate a focus on reducing disparities and signal that health equity is an important component of delivery system transformation.” Data collection and screening tools provide information to provide care and the social determinants of health (SDOH).
In 2016, Medicare added a new subset of Z codes after the implementation of ICD-10 coding. ICD-10 Z codes focus on social determinants of health with the intention to enhance quality improvement activities.38 Included as risk factors were such items as problems related to food insecurity, housing insecurity, transportation, child care, social isolation, and education, among others. Not specifically listed are access to digital health solutions, Wi-Fi, or cell services. Although the Z codes do not capture directly digital health equity and access data, they provide an opportunity for collection of data related to meeting these needs and ultimately their impact on care. Reports related to SDOH data could be part of a quality dashboard for executive leadership and Boards of Directors. This same data can be informative in identifying and meeting needs related to SDOH which can impact value-based care risk bearing arrangements.
Government Payers and Value-Based Care
The focus on social needs of individuals and the social determinants of communities has led Medicare and some state Medicaid programs to consider payment adjustments based on data collected in these areas. They also acknowledged the role telehealth will play in the future of those programs. On January 7, 2021, the Centers for Medicare and Medicaid Services (CMS) issued a roadmap for the states to address the social determinants of health under a value-based strategy. The new guidance describes how states can leverage existing flexibilities under federal law to tackle adverse health outcomes that can be impacted by social determinants of health to improve population health and reduce the cost of caring for high-risk populations. CMS acknowledges that an understanding of the social, economic, and environmental factors that affect the health outcomes of Medicaid and Children’s Health Insurance Program (CHIP) populations can change outcomes, including the use of digital solutions.
In the guidance, CMS acknowledged the importance of the services outlined being provided using telehealth modalities in addition to in-person visits. CMS went on to say that “states are strongly encouraged to assess their telehealth frameworks to determine if there are unnecessary restrictions preventing maximum utilization of telehealth for the services appropriate to be delivered via telehealth.” Although this issue was identified, the specific factors and solutions related to digital health equity were not specifically addressed in the guidance.
Actions to Improve Digital Health Equity
There are many ways for health care providers, technology companies, and their attorneys to be proactive in improving digital health equity.39 These are discussed below along with examples of efforts being taken in the health care field today to close the digital divide.
Make a Commitment and Be Intentional
As a starting point, health care providers and technology companies must intentionally commit to designing and implementing strategies in a way that all patients can access and understand. For example, CommonSpirit has embedded health equity and digital health equity into their strategy.40 The system includes questions related to technology access and digital health literacy in any process designed to evaluate digital solutions.41
While this commitment is critical, it is also important that digital health equity remain an intentional part of the conversation throughout the design, implementation, and evaluation stages of a digital solution. Health care providers and technology companies can partner to engage diverse groups, including those from historically marginalized communities, in the design and implementation of digital solutions.
To evaluate progress on implementation, health care and technology providers must understand their patients and the populations they are serving—including who is accessing and using digital solutions. CommonSpirit looks at data around the use of technologies. The health system stratifies this data by race, ethnicity, and social vulnerability to determine which communities are engaging in GetWell Docent, a program to provide culturally competent navigators embedded in the communities they serve. They quickly found through this process that they needed to not only provide docents who could speak the right language, but for some Spanish-speaking populations in California, it was also important for the docents to speak the right dialect.42
Improving Digital Health Access
There are many ways to improve digital health access. The provision of technology to patients and physicians is one way to improve digital health access when done in compliance with federal and state laws, including those discussed above. For example, when launching its Diabetes Telehealth Network pilot program, the University of Mississippi Medical Center provided patients participating in the program with tablet computers at no cost.43 Patients were then able to take and report their own vital signs daily, which led to improved patient outcomes, increased medication management, and participation in telehealth visits.44
Health care providers and technology companies can also proactively select solutions that minimize barriers to access. When Boston Medical Center (BMC) was selecting a remote patient monitoring solution to improve postpartum hypertension, the health system evaluated a variety of solutions. The team at BMC recognized that while a majority of their patients had access to smartphones, there was a divide in patients’ ability to connect—either they did not have consistent access to Wi-Fi or a data plan that could be used to support a video framework. As a result, BMC selected Rimidi because it uses the local cellular network that was accessible to all individuals with access to a smartphone.45
Health care providers and technology companies must also acknowledge that digital solutions may not be the best way to meet patients where they are on the digital continuum. One popular alternative is using mobile technology, or text messages, to provide information and an access point for patients to connect with health care providers. Research indicates that 90% of text messages are read within 90 seconds of when they are received.46 So while there are confidentiality and privacy laws to consider, texting is a powerful way to reach patients with the right message and ensure that the message is read at the right time.
There are other benefits to texting as well. It can be done in different languages so that messages can be adapted to cultural and linguistic attributes of populations. Texting also is relatively cost effective. Texting can be done in an interactive way, using two-way SMS systems to triage patient needs, provide timely information, and improve patient engagement.47
In addition, health care providers and technology companies can advocate for local, state, and national policy that would allow individuals to access digital health solutions while also strengthening health care providers’ capacity and ability to provide solutions in a way that individuals can understand. For example, at the national level, the AHA is advocating for investments in infrastructure, including broadband access, and for increased federal funding, coverage, and reimbursement for the expanded use of telehealth, broadband, and new technologies.48
Improving Digital Health Literacy
There are also ways to improve digital health literacy. Health care providers and technology companies can work together to design digital solutions that take into account patients’ situations and communication preferences. This involves asking patients what they want—including how they want to engage with these solutions or communicate with their care team—in order to design solutions that can and will be accessed.
That includes developing digital solutions that are linguistically and culturally sensitive and inclusive. Providence St. Joseph developed Circle, acquired by Wildflower, which provides information and resources to patients from pregnancy through delivery. As they designed this solution for their Spanish speaking population, rather than simply translating the language into Spanish, they evaluated the functionality of the app and asked, “how would a Spanish speaking individual approach the app?”49 As a result, they landed on a solution that was easier to utilize for this population.
These solutions can also be tailored to meet the needs of those with lower digital literacy, for example, by using more videos to ensure that patients of all literacy levels can access the information, or by using images, emojis, and symbols to help communicate messages. In addition, those with low digital literacy may be afraid to use technology or to trust their providers. To address these concerns, health care providers can increase engagement and trust by offering training to patients. For example, Ochsner Health launched an O Bar, which carries physician recommended digital products and is staffed by a full-time technology specialist who can help patients choose the right digital technology and provide setup guidance and support.50 During the pandemic, Nemours Children’s Health redeployed staff as digital health navigators to help patients and their families complete digital forms, troubleshoot connectivity issues, and better engage in telehealth visits.51
Organizations can also develop workflows that better allow clinical teams to engage with diverse patients through these digital tools. Froedtert & The Medical College of Wisconsin have implemented Babyscripts™, a platform designed to better connect expectant mothers with their doctors and resources to improve perinatal outcomes. Expectant mothers are invited to join Babyscripts™ after it is determined that they are pregnant. However, to ensure that all patients have the opportunity to utilize this solution, the care team at Froedtert proactively reaches out to those individuals who do not accept the invitation to encourage them to join.52
Conclusion
This is a critical time in health care. The COVID-19 pandemic highlighted that the adoption of technology is imperative for the future of health care delivery. As a result, understanding digital health equity is fundamental to health care. Both attorneys and health care leaders can play a significant role in the design and implementation of these solutions to ensure individuals and communities are able to access and engage with these solutions.
Steps Attorneys Can Take to Improve Digital Health Equity
-
Understand the legal and regulatory framework driving social determinants of health, health equity, and specifically digital health equity.
- Proactively help your clients understand digital health equity and legal issues that must be addressed when designing or implementing digital solutions.
- Help build partnerships with technology providers to ensure that digital health equity is included in the original design process, including through due diligence and contract negotiations.
- Educate technology providers to understand the legal considerations of health care providers when contracting with them.
- Review technology development, sales, and purchase agreements with an eye on health outcomes for all users and with culture competency, including those populations who are underserved.
- Educate yourself regarding biases in the health system and your own bias to understand how digital health and artificial intelligence can eliminate or perpetuate biases in data, development, and uses of digital health.
- Hire, promote, and support diversity at all levels of the organization, from your department or firm, the board, leadership, developers, and those providing care and services to patients.
- Ask good questions, think through problems, and consult with others to get a diversity of perspectives.
Author Profiles
Priya Bathija is vice president of Strategic Initiatives for the American Hospital Association. In that role, she leads AHA’s efforts to guide hospitals as they promote value and affordability by implementing strategies that improve outcomes, lower costs and enhance patient experiences. She also leads the organization’s work on maternal and child health, social determinants, and is a member of AHA’s Health Equity Strategies team. Formerly, Priya served as AHA’s policy expert on inpatient payment, graduate medical education, rural hospital issues, and spearheaded the AHA’s exploration of innovative delivery and payment system reforms to ensure access to essential health care services in all communities across the country. Prior to joining AHA, she served as hospital counsel for MedStar’s Georgetown University Hospital and Washington Hospital Center and as associate general counsel at ProMedica Health System. She started her career as an associate at Buckingham, Doolittle & Burroughs LLP. Contact her via email at [email protected].
Sarah E. Swank is a health care attorney in the Washington, DC office of Nixon Peabody LLP with more than 20 years of experience in both in the role of senior in house counsel in two large national health systems and as a strategic thought leader and advisor in nationally recognized, top-rated law firms. Sarah advised some of the first ACOs and national and international telehealth programs in the country. She is passionate about supporting clients navigating a complex and changing regulatory landscape to promote innovation and thoughtful growth through the compliant development of programs which provide equitable care. Sarah is a frequent national author and speaker for such organizations as AHLA, ATA, HCCA and ABA; Vice Chair of Education for the AHLA In-House Practice Group; Vice Chair of ABA Health Section Publication Board, and a key member of the Nixon Peabody Coronavirus Response Team. Contact her via email at [email protected].
1 Jonathan P. Weiner et al., In-Person and Telehealth Ambulatory Contacts and Costs in a Large US Insured Cohort Before and During the COVID-19 Pandemic, 4 JAMA
2 Wyatt Koma et al., Medicare and Telehealth: Coverage and Use During the COVID-19 Pandemic and Options for the Future,
3 Oleg Bestsennyy et al., Telehealth: A quarter-trillion-dollar post-COVID-19 reality?,
4 Disparities,
5 Paula Braveman et al., What is Health Equity?,
6
7 Allison Crawford, Digital Health Equity and COVID-19: The Innovation Curve Cannot Reinforce the Social Gradient of Health,
8 Jorge A. Rodriguez et al., Digital Health Equity as a Necessity in the 21st Century Cures Act Era, 323 JAMA 2381 (May 8, 2020).
9 Social determinants of health (SDOH) are defined as the conditions in the environments where people are born, live, learn, work, play, worship, and age that affect a wide range of health, functioning, and quality-of-life outcomes and risks. See Social Determinants of Health,
10 Homework Gap and Connectivity Divide,
11 Mapping Broadband Health in America 2017,
12 Arnesa A. Howell, Why achieving digital equity is a critical challenge of our time,
13 Societal Factors That Influence Health,
14 Fourteenth Broadband Deployment Report,
15 Shelley McKinley, Microsoft Airband: An annual update on connecting rural America,
16 Eduardo Porter, A Rural-Urban Broadband Divide, but Not the One You Think Of,
17 Michael Martin, Computer and the Internet Use in the United States: 2018 (Apr. 21, 2021),
18 Internet/Broadband Fact Sheet, Pew Research Center, Apr. 7, 2021, https://www.pewresearch.org/internet/fact-sheet/internet-broadband/ (last visited Apr. 22, 2022).
19 Mobile Fact Sheet,
20 Eric T. Roberts & Ateev Mehrotra, Assessment of Disparities in Digital Access Among Medicare Beneficiaries and Implications for Telemedicine, 180
21 Courtney R. Lyles et al., Focusing on Digital Health Equity, 326 JAMA 1795 (Oct. 22, 2021).
22 Id.
23 Coronavirus Preparedness and Response Supplemental Appropriations Act of 2020, Pub. Law No. 116-123, 134 Stat. 146 (2020). See also Coronavirus Aid, Relief, and Economic Security Act, Pub. Law No. 116-136, 134 Stat. 281 (2020).
24 For example, the Centers for Medicare and Medicaid Innovation (CMMI) has expanded telehealth waivers as part of their evolving payment models. For example, the Next Generation ACO Telehealth Expansion Waiver eliminated the rural geographic component of originating site requirements and allows the originating site to include a beneficiary’s home. In addition, it expanded the provider types that could use asynchronous telehealth services. See Next Generation ACO Model Telehealth Expansion Waiver (2021), https://innovation.cms.gov/files/x/nextgenaco-telehealthwaiver.pdf.
25 Section 1128A(a)(5) of the Civil Monetary Penalties Act (CMP) provides for the imposition of civil monetary penalties against any person who offers or transfers remuneration to a Medicare or state health care program (including Medicaid) beneficiary that the benefactor knows or should know is likely to influence the beneficiary’s selection of a particular provider, practitioner, or supplier of any item or service for which payment may be made, in whole or in part, by Medicare or a state health care program (including Medicaid). “Remuneration” for purposes of the CMP includes “transfers of items or services for free or for other than fair market value.” Section 1128A(i)(6). For purposes of the Beneficiary Inducements CMP, the term “remuneration” does not apply to “remuneration which promotes access to care and poses a low risk of harm to patients and federal health care programs also known as the “Promotes Access to Care Exception.” 42 C.F.R. § 1003.110 (2022). See also, OIG Advisory Opinion 22-08 (regarding an arrangement whereby certain existing patients use limited-use smartphones loaned to such patients to facilitate access to telehealth services).
26 42 U.S.C. § 1320a-7b(b) (2021) (prohibits offering, paying, soliciting, or receiving anything of value to induce or reward referrals or generate federal health care program business).
27 Id. § 1395nn (prohibits a physician from referring Medicare patients for designated health services to an entity with which the physician (or immediate family member) has a financial relationship, unless an exception applies).
28 Some loaner programs may fit under the Promotes Access to Care Exception if they would improve a beneficiary’s ability to obtain items and services payable by Medicare or Medicaid. In addition, the remuneration must pose a low risk of harm by (i) being unlikely to interfere with clinical decision making, (ii) being unlikely to increase costs to federal health care programs or beneficiaries through overutilization or inappropriate utilization, and (iii) not raising patient safety or quality-of-care concerns. 42 C.F.R. § 1003.110.
29 See, e.g., OIG Advisory Opinion No. 19-02 (Jan. 24, 2019), https://oig.hhs.gov/documents/advisory-opinions/759/AO-19-02.pdf (pharmaceutical manufacturer’s proposal to loan, on a temporary basis, a limited-functionality smartphone to financially needy patients who do not have the technology necessary to receive adherence data from a sensor embedded in a prescribed antipsychotic medication).
30 See Title VI of the Civil Rights Act of 1964 (42 U.S.C. § 2000d) and its regulations (45 C.F.R. pt. 80) (prohibits discrimination on the basis of race, color, or national origin), Section 504 of the Rehabilitation Act of 1973 (29 U.S.C. § 794) and its regulations (45 C.F.R. pt. 84); the Age Discrimination Act of 1975 (42 U.S.C. § 6101) and its regulations 45 C.F.R. pt. 90. For more information, see Laws and Regulations Enforced by OCR,
31 Americans with Disabilities Act of 1990, Pub. L. No. 101-336, 104 Stat. 328.
32 For current information about the ADA see Celebrating the Americans with Disabilities Act,
33 Letter from Jocelyn Samuels, U.S. Dep’t of Health & Hum. Servs., Off. for Civ. Rts., to Colleagues, Guidance and Resources for Electronic Information Technology: Ensuring Equal Access to All Health Services and Benefits Provided Through Electronic Means, at 2 (Dec. 21, 2016), https://www.hhs.gov/sites/default/files/ocr-guidance-electronic-information-technology.pdf.
34 Title VI of the Civil Rights Act of 1964 (requires recipients of federal financial assistance to take reasonable steps to make their programs, services, and activities accessible by eligible persons with limited English proficiency). For more information, see Limited English Proficiency (LEP),
35 See, e.g., including those recommended by the Deaf/Hard of Hearing Technology Rehabilitation Engineering Research Center, About the DHH-RERC,
36 Studies of telehealth accessibility during the COVID-19 pandemic have led some to conclude that “the pandemic’s widespread disruption of American life caused broader, unexpected consequences for people with disabilities.” Blake E. Reid et al., Telehealth and Telework Accessibility in a Pandemic-Induced Virtual World,
37 Social Risk Factors and Performance in Medicare’s Value-Based Purchasing Program,
38 See CMS,
39 Jorge A. Rodriguez et al., Digital Health Equity as a Necessity in the 21st Century Cures Act Era, 323 JAMA 2381 (2020).
40 Advancing Health, Seven in Seven: Digital Solutions for Perinatal Care ft. CommonSpirit Health,
41 Id.
42 Id.
43 University of Mississippi Medical Center–Jackson: Remote Patient Monitoring Program,
44 Id.
45 Advancing Health, Seven in Seven: Digital Solutions for Perinatal Care ft. CommonSpirit Health,
46 Sandeep Puri, Digital Health for Rural Healthcare,
47 Lisa Fitzpatrick et al., The Digital Divide in Healthcare: It’s Not Just Access, HIMSS (Feb. 4, 2021), https://www.himss.org/resources/digital-divide-healthcare-its-not-just-access.
48 2021 AHA Advocacy Agenda,
49 Advancing Health, Seven in Seven: Digital Solutions for Perinatal Care ft. CommonSpirit Health,
50 O Bar,
51 Sara Heath, Is the Digital Divide the Newest Social Determinant of Health?,
52 Advancing Health, Seven in Seven: Digital Solutions for Perinatal Care ft. CommonSpirit Health,