Staffing Shortages: Responses and Risks at Hospitals and Health Systems
This Briefing is brought to you by the Enterprise Risk Management Affinity Group of AHLA’s Hospitals and Health Systems Practice Group.
- January 27, 2022
- Don A. Briones , ECG Management Consultants
Although it’s tempting to blame the pandemic for today’s health care staffing shortage, the crisis is not a new one. For example, in the wake of the recession from December 2007 to June 2009:
- Hospitals saw a significant number of nursing vacancies that required them to pay premiums and improve working conditions.
- Physicians encountered significant burnout that compelled many to leave their practices.
- Nonclinical workers gravitated toward high‑tech and other industries for better pay.
But while the roots of the current crisis precede the pandemic, there’s no denying that COVID-19 has made matters much worse. This article examines the health care workforce situation since March 2020, the risks that organizations face as they struggle to offset the impact of health care workers leaving the profession, and mitigating strategies that respond to staffing shortages.
Staffing Shortage Situation
When the pandemic began in early 2020, the industry faced significant declines in volume due to the mandated cancellations of elective surgeries; safety concerns about contracting COVID‑19; lack of available child care; and in many markets, capacity constraints because of supply shortages and space needed to treat COVID‑19 cases. Between March and June 2020, volume declined to 60% of pre-pandemic levels.[1]
The decline in volume resulted in massive financial losses for hospitals and health systems, and many decided to furlough or lay off staff to help offset their low financial performance. As organizations started to see gradual increases in the demand for services and received supplemental relief funds from the CARES Act and other sources, they eliminated the furloughs and rehired staff, but in an environment that had changed dramatically since before the pandemic. Providers and nurses were caring for patients under highly difficult workplace conditions, and many nonclinical staff were forced to work remotely.
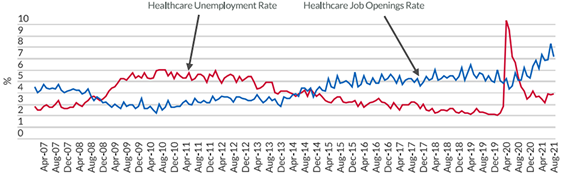
Nevertheless, many health care workers began returning to the workforce to fill open positions. They now have ample opportunities, as the demand for staff continues to grow, decreasing the unemployment rate to as low as 3% to 4% from a high of over 10% in spring 2020, as shown in figure 1.
Figure 1. Unemployment Rate versus Job Openings Rate: Healthcare[2]
Despite the low unemployment rate, many organizations are still experiencing a high level of job vacancy due to workers deciding not to return or current employees leaving their positions. In a recent health care workforce report,[3] the turnover rate at the end of 2020 increased 20% from 2016 to 19.5%, with nursing departures up 28% from 2016 to 18.7%. The report noted several key reasons for the increase in turnover:
- Career Advancement: Staff leave because they do not see opportunities for promotion, or they decide to get additional education and pursue advanced careers.
- Retirement: Many in the workforce are aging and deciding to retire instead of adapting to the new normal.
- Working Conditions: Staff continue to work overtime, and the patient care requirements due to COVID‑19 have resulted in higher levels of staff burnout.
- Pay: Staff are being recruited to other organizations or agency firms to work for higher pay, with wages that are at up to 50% higher than their current compensation. Others found opportunities to work from home, often for more pay than being on site.
- Regulatory Requirements: Staff turnover increased in states that mandated vaccination as a condition of employment, and higher turnover is expected when the CMS vaccination mandate takes place in early 2022.
These staffing issues have not gone unnoticed by industry observers. A recent article issued by Fitch Ratings[4] said the health care industry is facing long-term impacts, and organizations will need to find sustainable solutions to offset the negative financial and operational impacts of not having enough skilled staff to provide acceptable patient care. Otherwise, they will be considered a risk by the rating agencies.
Responses to Staffing Shortage Issues
Workforce shortages have become severe enough that organizations have made them a main focus area in mid- to long-range strategic planning efforts. Some of the strategies that hospital executives have considered include:
- Enhance employee retention programs and initiatives to slow the increase in employee turnover.
- Improve current wage compensation systems and practices.
- Enhance workforce processes and infrastructure.
- Design, implement, and optimize advanced technologies to simplify or eliminate redundant work.
- Increase the workforce supply through partnerships and other transactions.
While each of these strategies may have unique characteristics at any given organization, the common thread is the goal to keep employees satisfied at their current jobs, recruit to appropriate staffing levels to avoid service disruptions, and sustain these solutions to positively impact long-term financial and operational performance.
Employee Retention Programs and Initiatives
Hospitals and health systems have recognized the lost value in employee turnover. A study published in Becker’s Hospital Review in 2018 shows that the annual cost of a 1.0 FTE staff nurse vacancy at a medium-sized hospital can be as much as $175,000[5] (and is likely higher today). Organizations are reevaluating how they are connecting with their employees and looking for ways to boost their experience in the workplace. Some ideas that have been implemented include:
- Employee-centric program enhancements that provide active listening opportunities for management to respond to issues, concerns, and other matters that otherwise would lead to employee burnout or dangerous workplace situations.
- Tuition and student loan forgiveness incentives that give employees opportunities to obtain new skills.
- Programs designed to help managers become more empathetic to employees’ needs.
Wage Compensation Systems and Incentive Pay Practices
With increasing competition for labor resources, many hospitals and health systems are boosting their wages to compete with other organizations in their market or with agencies that are luring staff away with higher contract rates. In addition to conducting market-based wage compensation evaluations, hospitals and health systems are offering increasingly lucrative recruitment incentives. Sign-on, retention, and referral incentives are not new but are now being offered to a wider employee base. For example, prior to the pandemic, nurses usually received recruitment incentives due to the prolonged shortage. Now, these incentives are being offered to medical assistants, respiratory therapists, imaging technicians, and other nonnursing positions.
Workforce Process and Infrastructure Improvements
One of the early actions hospitals and health systems took was instituting tighter controls on how they use their labor resources.
- Because skilled workers are in such high demand, organizations are revising job descriptions and the work required so that each employee can operate to the top of their license and capacity can be aligned with the best available resources.
- Other organizations are increasing the flexibility of their workforce by revising their open positions to hire for the right mix of full-time and part-time staff. For example, a hospital may revise a full-time nurse job opening to a position for a part-time nurse and a full-time technician.
- Hospitals and health systems are also improving patient care and other processes by eliminating waste and simplifying work, making burdensome tasks easier to manage.
Advanced Technologies
At the beginning of the pandemic, hospitals and health systems accelerated the use of telehealth and other technologies to serve patients. From a labor resource perspective, organizations continue to examine the benefits of providing care in alternate settings using advanced technologies, with staff located remotely. Health care entities are exploring inpatient virtual care models that ease some of the burden of on‑site nurses by having remote nurses provide patient care via technologies that help distinguish between care that should be provided on site as opposed to virtually.
Hospitals and health systems also continue to refine costly electronic health record (EHR) systems to improve clinical productivity and efficiency. While the EHR can be credited with helping reduce clinical variation and improve outcomes, physicians and other clinicians must devote significant administrative time to reap the benefits of the investment, which often leads to provider frustration and burnout. Organizations are implementing system optimization strategies that tie workflow and system functionality closely, customize settings for physicians to access data more quickly, provide ongoing education and training for physicians, and establish a culture of resolving system issues in a timely and effective manner.
For administrative support functions, health systems are exploring the use of robotic process automation (RPA) to simplify, inform, and eliminate tasks. RPA is a technology currently used for back-office operations, specifically in revenue cycle and accounting operations, to eliminate repetitive processes and provide business intelligence through machine-learning capabilities that can enable decision-making in day-to-day operations and improve strategic management.
Partnerships and Other Transactions
Some organizations are developing private-public partnerships to resolve their labor resource issues. For example, many community hospitals are collaborating with local school districts and vocational schools to establish employee pipelines to develop certified skill sets for medical assistants and nurses, respectively. Additionally, hospitals that are in the same geographic region as other health organizations are looking to pool nursing and other clinical staff through joint ventures, acquisition, or formation of new companies (a practice that has long existed for nonclinical functions such as IT, HR, finance, and other management services).
Risks to Hospitals and Health Systems
The legal risks of addressing labor relations issues associated with staffing shortages continue to grow.
Organized Labor Activity
As many organizations mandate overtime and other extracurricular shift work, some caregivers are unable to comply with the directives and either leave the organization or seek assistance from labor relations organizations or unions to seek better working conditions. Organizations that cannot effectively address staff concerns often find themselves facing labor strikes or “sick out” situations, further complicating their ability to provide patient care.
Compensation Practices
Since many organizations made exceptions to their current wage compensation practices to retain and recruit employees, mismanagement of their compensation system may cause wage compression issues and increase the risk of workplace equity overall. As exceptions to an organization’s compensation pay policies increase, so does the risk of employees perceiving unfair compensation practices, which undermines the organization’s ability to demonstrate equity in the workplace. These exceptions need to be explored and possibly addressed to strengthen employment equity and mitigate unfair compensation practices.
Contract Labor
As the number of third-party relationships with contract labor vendors and agencies increases, hospitals need to pay greater attention to contractual details, since they are liable for the negligence of anyone who provides services at their sites. Organizations need to review their current liability insurance policy and terms and conditions, including malpractice, cybersecurity, and other pertinent insurances, as well as the current vendor contract arrangements for obtaining contract labor to ensure they are adequately covered.
Financial Risks
From a fiscal perspective, organizations face the risk of not achieving financial performance targets despite their investment in building a workforce management program. According to Fitch Ratings, the accelerating wages in recent months need to be sustained in the long term as job openings continue to increase, and the growing gap between these vacancies and the number of available workers produces a universal labor dislocation that cannot be fixed when volume returns to pre-pandemic levels.
The competition for labor resources between health care organizations, as well as contract agencies, produces a “wage war” effect, and staff then consider the most financially viable option for themselves. This gives employees the advantage, which drives labor costs even higher. It is this impact, along with the possibility of limited profitable services due to staff shortages, that generates a long-term risk for hospitals and health systems to receive rating agency downgrades.[6]
Also, the reduced availability of clinical workers and providers limits a hospital’s ability to serve patients, which generates lower levels of revenue.
Compliance with Vaccination Requirements and Other Regulations
Organizations also must face the possibility of complying with regulatory mandates. While CMS is currently suspending enforcement of the mandate that Medicare- and Medicaid-participating providers, suppliers, and their staff must be vaccinated, the possibility that this rule will eventually be enforced puts organizations that are unable to quickly fill vacancies at risk of having limited staff available to provide services. Continued labor shortages also result in staff working in challenging conditions, such as mandated overtime and other practices not favorable to employees, that may run afoul of the hospital’s employment policies or union collective bargaining agreements.
Moving Forward
The breadth and depth of organizational risk associated with the labor shortage has intensified during the pandemic and will likely continue after the crisis has subsided. Mitigating these risks will be a main driver in a hospital or health system’s ability to remain financially solvent and relevant in their market. Professionals who are involved in risk management, labor relations, and other risk-related disciplines will need to employ a combination of strategies and solutions such as those outlined above to respond to this ever-growing challenge. Hospitals and health systems that succeed in doing so will be employers of choice and be able to manage future risks effectively.
About the Author
Don A. Briones is senior manager at ECG Management Consultants, a health care consulting firm, and advises clients on performance improvement solutions, including strategic growth, finance transformation, and operational effectiveness. Don is a former CFO, Operational Finance Executive, and Corporate Compliance Officer for hospitals and health systems in the San Francisco Bay Area.
[1] “Early 2021 Data Show No Rebound in Healthcare Utilization,” Peterson‑KFF (Aug. 17, 2021), https://www.healthsystemtracker.org.
[2] US Bureau of Labor Statistics (Sept. 2021).
[3] 2021 NSI National Health Care Retention & RN Staffing Report, NSI Nursing Solutions, Inc.
[4] “Non-for-Profit Healthcare Staffing Shortage Has Long-Term Effects,” Fitch Ratings (Oct. 27, 2021).
[5] “RN Recruitment: The Cost of Doing Nothing Is Costly,” Becker’s Hospital Review (Aug. 31, 2018).
[6] “Rising Labor Expenses Cloud U.S. NFP Hospitals’ 2022 Outlook,” Fitch Ratings (Dec. 7, 2021).